
A medical professional provides practical and proven advice to assist you in achieving and sustaining effective weight loss.
Managing weight with type 2 diabetes can pose distinct challenges; however, with appropriate support, it can become a journey that results in significant enhancements in health and well-being.
Dr. Jennah Siwak, a board-certified obesity specialist recognized by many in the GLP-1 medication community on TikTok as @WeightDoc, tackles this challenge with a combination of evidence-based medicine, empathy, and realism.
In this guide, Dr. Siwak outlines how she aids patients in navigating weight loss for improved health outcomes, focusing not only on the scale’s numbers but also on preventing complications such as kidney disease, heart disease, and neuropathy.
The quality of nutrition is more significant than the diet label.
Dr. Siwak clarifies, “There is no research-proven ‘best’ diet or ‘best’ macronutrient pattern for individuals with diabetes.”
Rather than pursuing trends, she stresses the importance of enhancing the quality of one’s diet. This involves constructing meals that include:
non-starchy vegetables
fruits
legumes
whole grains
nuts
seeds
Additionally, it entails reducing the intake of:
red meat
sugar-sweetened beverages
refined carbohydrates
ultra-processed foods
Diets such as the Mediterranean and DASH diets are frequently recommended due to their benefits for heart health. Dr. Siwak states, “Diabetes and obesity are risk factors for heart disease,” which is why she often advocates for a heart-healthy diet. These dietary patterns contribute to lowering blood pressure, cholesterol levels, and overall cardiovascular risk.
However, sustainability is essential. “The most effective dietary approach for weight loss is the one that can be maintained over time,” she states. A restrictive regimen, even if it guarantees quick outcomes, is not beneficial if a patient cannot adhere to it in the long run.
To ensure that nutrition is genuinely tailored to the individual, Dr. Siwak often recommends that patients consult registered dietitians. “Meal plans ought to be personalized and are most effectively created by a registered dietitian who has expertise in diabetes and obesity management.”
Sleep plays a crucial role in managing weight and blood sugar levels.
People frequently underestimate the influence of sleep on weight and elevated blood sugar. “Sleep has been associated with weight,” Dr. Siwak observes. Inadequate sleep or unresolved sleep disorders, such as obstructive sleep apnea (OSA), can interfere with hormones that regulate appetite, including leptin and ghrelin.
“Insufficient sleep is linked to low leptin (which decreases feelings of fullness) and high ghrelin (which increases hunger),” she explains.
Chronic sleep deprivation can lead to fatigue, diminishing the motivation to engage in physical activity, thereby creating a cycle that exacerbates both weight and glucose management. Tackling sleep-related issues, including screening for OSA, can be an essential component of an effective weight loss strategy.
GLP-1 medications represent only one aspect of treatment.
GLP-1 receptor agonists such as Ozempic, Wegovy, and Mounjaro can serve as significant allies for individuals managing both type 2 diabetes and obesity.
“GLP-1s can be an excellent resource,” Dr. Siwak states, emphasizing that they reduce appetite by delaying gastric emptying (the speed at which food exits the stomach and enters the intestines) and by signaling satiety (fullness) to the brain.
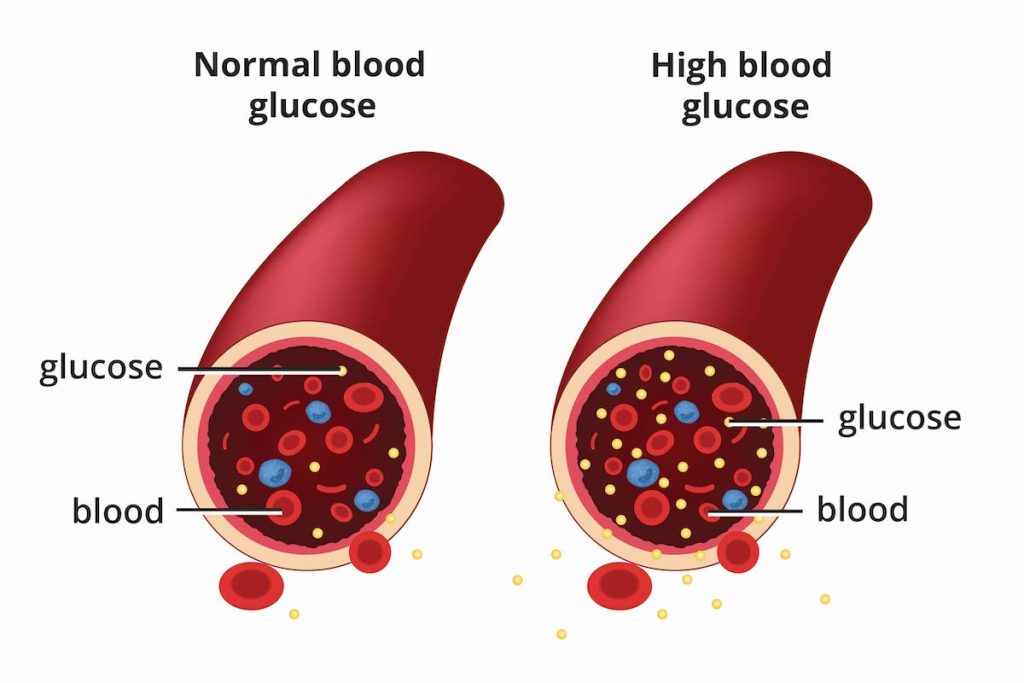
“Additionally, they offer glycemic control (aiding in the stabilization of blood sugar levels) through their effects on the pancreas, which enhances our bodies’ ability to process glucose more effectively.”
However, it is important to note that medications are not a cure-all. Lifestyle and behavioral modifications are essential, and medications should be viewed as a component of a holistic treatment strategy rather than a replacement for these changes.
Mental health support is crucial, not merely optional.
Navigating a new diagnosis such as type 2 diabetes or undergoing a significant physical change through weight loss can elicit a variety of emotional reactions. While some individuals may feel an increase in confidence due to weight loss, others may feel disappointed when weight loss does not resolve all their concerns.
“Frequently, the belief is, ‘If I can JUST lose the weight, EVERYTHING will improve,’ but it becomes evident that weight loss does not enhance every aspect of life,” Dr. Siwak explains. This emotional disparity can even result in a decline in mood or persistent body image challenges.
Stress is another critical element that can disrupt healthy behavior modifications. It can influence sleep, eating habits, and overall motivation, making it more difficult to maintain consistent healthy practices.
Tackling stress through mental health support, self-care strategies, and setting realistic goals can lead to significant improvements.
She underscores the necessity of processing these feelings with assistance. “I often refer to our therapist and counselor colleagues in behavioral health,” she notes. A robust support network, whether through friends, family, or community organizations, can also aid individuals in adhering to lifestyle modifications.
Progress may be gradual, and that is not necessarily a negative aspect.
Managing expectations is among the most effective strategies employed by Dr. Siwak with her patients. “Avoid comparing yourself to individuals who are sharing their weight loss experiences online,” she cautions.
Quick weight loss is not sustainable and may result in adverse effects such as muscle loss, fatigue, and hair thinning.
“Ideally, we aim for individuals to lose no more than 1% of their body weight each week,” she states. This typically equates to a loss of 1 to 2 pounds weekly. Furthermore, gradual progress often results in more favorable long-term outcomes.
She motivates her patients to concentrate on non-scale achievements: enhancements in laboratory results such as A1C, glucose, cholesterol, and even normalized liver enzymes. These indicators reflect an improvement in health, even if the scale does not show rapid changes.
Progress may be gradual, and this is not necessarily a negative aspect.
One of the most impactful strategies employed by Dr. Siwak with her patients is managing their expectations. She cautions, “Avoid comparing yourself to individuals who are sharing their weight loss experiences online.”
Quick weight loss is not sustainable and may result in adverse effects such as muscle depletion, exhaustion, and hair thinning.
“Ideally, we aim for individuals to lose no more than 1% of their body weight each week,” she states. This typically equates to a loss of 1 to 2 pounds weekly. Furthermore, gradual progress often results in more favorable long-term results.
She motivates her patients to concentrate on victories that are not reflected on the scale: enhancements in laboratory results such as A1C, glucose, cholesterol, and even normalized liver enzymes. These indicators signify that health is improving, even if the scale does not show rapid changes.
Each individual’s experience with diabetes is unique.
Early interventions tend to be more beneficial for patients who have recently been diagnosed, as their insulin resistance may not yet be significantly pronounced. However, for individuals who have been living with type 2 diabetes for an extended period, Dr. Siwak stresses the importance of establishing achievable goals.
“In type 2 diabetes, there is a gradual deterioration in the functionality of the pancreatic beta cells,” she clarifies. This indicates that weight loss may not completely eliminate the necessity for medication, particularly if the condition has persisted for many years. “She adds, ‘Losing weight will not necessarily eliminate the requirement for diabetes medications.'”
This truth can be disheartening, yet it does not imply that efforts are in vain. Even a slight reduction in weight can lead to improvements in blood sugar levels, lower cardiovascular risk, and a better quality of life.
Diabetes is not your fault
One of the prevalent misconceptions that Dr. Siwak encounters is the belief that type 2 diabetes is solely a consequence of poor lifestyle choices. “Most individuals with type 2 diabetes have a family history,” she states. “There is a significant genetic factor involved in diabetes.”
She clarifies that genetics functions as the “lock,” while lifestyle serves as the “key.” Although healthy habits can postpone or lessen the severity of diabetes, they cannot always completely avert it. Holding yourself accountable for a diagnosis is not only emotionally distressing but is also frequently rooted in misunderstandings regarding the actual causes of type 2 diabetesTrusted Source.
Takeaway
Managing type 2 diabetes through weight loss, if that is medically advised for you, is not about discovering the ideal diet or medication. As Dr. Jennah Siwak articulates, “Show yourself grace! Losing weight is genuinely challenging, and we understand it can be even more arduous for individuals with metabolic diseases, such as type 2 diabetes.”
A sustainable and compassionate strategy that integrates nutrition, mental health support, medical resources, and lifestyle modifications is the most effective way forward, and it should be tailored at every stage.
HEALTH